How to Stay Covid Safe When in Hospital
A guide to navigating the risk of hospital acquired Covid - as well as how to manage overall risk of nosocomial infections and hospital derived complications.
A few weeks ago I wrote an article about how a large number of disabled and chronically ill people won’t go to the ER unless they think they’re literally dying. The responses I got showcased just how many people are rightfully afraid of the hospital. Many asked for tips to make trips easier - and it quickly morphed into a series of posts designed to help people adapt to the realities of hospital care when you’re chronically ill. You can find the original post here, and Part 2 ‘Tips for Surviving a Hospital Trip When Chronically Ill’ here.
Today I want to talk about the risk of Covid infection when in an ER or hospital setting. Hospital Acquired Infections (also called Nosocomial Infections) have always been a concern of mine given my poor health and struggling immune system. More often than not if I go to the hospital I end up coming out sick with some kind of virus or bug. I began masking in hospital settings a few years before Covid - but even I wasn’t prepared for how hard it would be to navigate hospital settings during a pandemic.
No one should ever have to risk their health to get necessary medical care. People shouldn’t feel like it’s a choice between care and Covid. Yet many hospitals have all but given up attempting to prevent its spread - leaving vulnerable patients on their own to prevent infection.
Nosocomial Covid infections have a much higher fatality rate than those acquired in community settings. This journal article placed it at 8.4% while this article from Australia said almost one in ten patients who caught Covid in hospital died from the disease.
Many of us do whatever we can to avoid needing the hospital - but if you’re forced to go - what should you do in order to give yourself the best odds of avoiding infection?
In my opinion the most important thing you can do is wear a good quality fitted respirator. An N95 or better that has a tight seal on your face. There are a variety of DIY fit tests you can do and if you think you may be in the hospital regularly - they’re worth doing to ensure you’ve got the best protection available. For most people a headstrap mask gets a better fit than an earloop - but every face is different and it’s worth experimenting. I wear the Vitacore N99 headstrap respirator - though I know many people who use an elastometric like the Flo Mask or a P100 half face respirator. Remember - the best mask is the one that fits your face and that you will wear. If it’s too uncomfortable and you’re constantly taking it off - it won’t give you much protection. Try some out and find what works for you!
Image Description: A picture showing a white Vitacore N99 headband respirator beside a white and red box of 10 respirators.
Respirators can be expensive - and most hospitals will only provide surgical masks (if they provide any at all). There are some great organizations and Mask Blocs that will provide free respirators to people who can’t afford them. In Canada I highly recommend Donate a Mask - they have an online store where you can purchase a wide variety of masks and they also give masks to people who can’t afford them. If you’re not in Canada you can use this site to find a mask bloc in your local area.
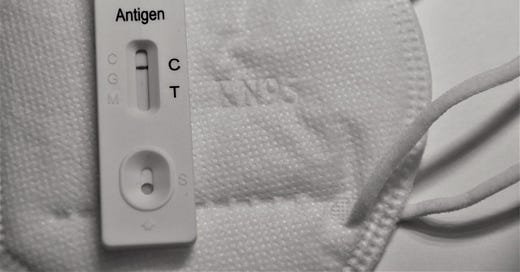
Image description: A white SARS-Cov-2 rapid test sits on top of a white respirator.
I also recommend taking a Covid test before going to the hospital. Get a date and time stamped photograph of the result so that you know your status before going in. If you’re infected in hospital and ever need to prove it - this will help.
Other things you can do in hospital to protect yourself include bringing an air purifier and a CO2 monitor. The CO2 in a room can help determine how well they’re ventilating the air. We know Covid is airborne - so you can be infected even if no one else is in the room. A low CO2 reading doesn’t necessarily mean a room is ‘safe’ but it is a strong indication that it is ‘safer’. There’s also new research coming out to indicate that Covid is more infectious at higher CO2 levels - so a lower level is a good indicator of reduced risk.
There are many CO2 monitors on the market - the one I see most commonly used is the Aranet. Generally speaking a CO2 reading less than 600 is a good indication that the space is well ventilated. I don’t remove my mask if anyone is sharing the room with me and/or nearby…. but if I need to remove it to drink or take medications I will wait until I see a low CO2 reading and no one is near me. Near field transmission is a risk regardless of how low the CO2 is - so if someone is close by it’s best to keep your mask on.
If you have to remain in hospital you may want to bring an air purifier you can use in your room. Air purifiers are also a great way to reduce household transmission and cut the amount of dust, pollen and other allergens in your home. If you’re not familiar with Corsi Rosenthal boxes - they’re a fun and easy way to DIY your own air purifier. They might be a bit big for hospital use - but there are many smaller HEPA filters on the market. One I frequently see used in hospital settings is the Levoit core mini.
Image Description: A White Corsi Rosenthal box with furnace filters and white box fan. Image courtesy of Clean Air Crew.
There are many engineers and companies working hard to develop new and improved products to help reduce the risk of Covid in all kinds of situations. One such product is a laminar flow purifier like this one by Adam Wong which can be purchased on Amazon. It is a small purifier that directs filtered air towards your face - ensuring the air doesn’t mix with other air within the room. Products like this are a great extra layer of protection for circumstances where you might be forced to remove your mask.
Another product that can help reduce risk are Far UV devices. These are small portable UV lights that can kill viruses in the air. They’re not legal in all countries and the technology is still relatively new - but I’ve seen many high risk patients take them into hospital settings. Pictured below is a set of four Far UV torches by Nukit. I highly recommend researching the safety of any Far UV product you may be considering - as well as the laws in your country to ensure they’re permitted. I’m excited to see where technology takes us - and thrilled there are so many people designing products to help us be safer.
Image Description: A set of 4 Far UV torches in a carrying case. They can be found at the Cyber Night Market - photo courtesy of Nukit.
Other tools that can provide additional layers of protection are things like CPC mouthwashes and certain nasal sprays. If you can’t tolerate commercial mouthwashes and nasal sprays - saline rinses can help. They may not kill the virus but they can help flush it out and reduce viral load. In a situation like a hospital stay where it might be impossible to avoid exposure to viruses - anything you can do to reduce the amount of virus in your body will help. I do a saltwater gargle three times a day (which also helps with my dry mouth and ulcers) and others have said that they use a Neti Pot with success.
Speak to the staff at the hospital and see if you can come to an arrangement where healthcare workers who are treating you will be required to mask. You can do all the things I’ve listed in this article - but if you’re being treated by someone who is Covid positive, the BEST protection is for them to wear a mask. Source control drastically reduces infectivity and two way masking is more effective than one.
This is becoming harder and harder to accomplish - but if possible ask to speak to a nurse floor manager or a patient relations representative, explain your concerns and offer to provide masks if they don’t have any. Consider placing a sign on the door that says ‘Masks Required for Entry’ along with spare masks.
The sad reality is that until governments, public health and hospitals start taking airborne precautions seriously - it will be increasingly difficult to protect ourselves from Covid in hospital settings. The continued emphasis on droplet dogma and handwashing, combined with the attitude that Covid is over/mild has led most people to believe additional mitigations aren’t worth the effort. Many staff members are working while sick which unfortunately puts patients at risk, and others refuse to acknowledge that asymptomatic spread is real and far from rare.
The good news about these mitigations is they will also protect you from other hospital acquired infections, thereby increasing the odds that you don’t leave the hospital sicker than when you came in. Every layer you use reduces risk - so use whatever you can access and don’t be afraid to advocate for yourself.
Finally - I want to recognize that virtually all mitigations cost money. The high cost of these items highlights one of the biggest issues with the pandemic - equity and social justice. Protection is only available to people privileged enough to afford it - while others are being left behind. Even in a hospital setting - if you’re marginalized or a person of colour you may have a harder time getting staff to take precautions or allow you to use protection you’ve brought from home.
Until we acknowledge and address these inequities - Covid will continue to be a significant threat to everyone. All people who want and need to protect themselves should be able to do so. It shouldn’t be a privilege afforded only to the most affluent among us.
If you’re in a position of privilege - please consider donating to a mask bloc in your area. Help lobby goverments and public health to provide free masks and tests to anyone who needs them. Help us fight for clean air benchmarks in public spaces. Educate your local hospital on the need to prevent hospital acquired Covid. If you’re showing up at the hospital with all these tools to keep yourself safe - consider telling staff that there’s many people who can’t access those tools and are relying on the healthcare workers to mask up as their only form of protection.
Together we can drastically reduce the spread of Covid in hospitals - and in doing that we will reduce overall nosocomial infections as well. But like everything else in life - this is a problem that won’t be solved until we acknowledge its existence. Please consider sharing this article with healthcare workers you know, or with friends and family who may not understand the high risk of infection in hospital settings. Together we can make a difference and make hospitals safer for everyone.
If you’re not already subscribed - you can subscribe for free below to make sure you don’t miss the rest of the series! Part 4 ‘How to be an Effective Advocate for a Disabled Patient’, and Part 5 ‘My Most Dangerous ER Experience and How My Advocate Saved My Life.’
Did I miss anything? What tips and tricks have you used to avoid getting sick while in hospital? Please leave a comment to help others in the community find the best ways to protect themselves.
Disclaimer: I’m not being sponsored or financially compensated by any of the products mentioned in this article. I’ve provided links so that readers can see exactly what products I personally use and/or have witnessed others use with great success. If you have questions about any of the products included in this article - feel free to leave a comment or send me a message and I will try and help!







Thank you so much for this post. In the event it encourages someone to try, I recently had surgery, an overnight hospital stay and a successful experience requesting masking. I spoke with my surgeon beforehand and on the day of, telling her it was important to me that I be masked before I left the operating suite and was wheeled back to my room. I run a small business and impressed upon her the negative financial fallout I’d experience from getting sick in addition to negative impact on my health. (Idk if this extra reason helped but I was willing to say anything to persuade people.) She agreed to help me and assured me masks were mandatory in the OR, though I saw them in baggy blues when I got there. I had the same conversation w my anesthesiologist and nurse anesthetist the morning of. Everyone agreed. When I came to in the recovery room my mask was on and I kept it on until I left. I also used a Levoit air purifier in my room (thankfully, a single) and kept the door closed. I asked the nurses if they’d wear a mask. They agreed but wouldn’t have worn one if I hadn’t asked. Everyone was cooperative. My procedure took place in suburban Philadelphia, a city where a small minority of people never stopped masking and I’ve never seen anyone hassled about it. That said, almost no one in the hospital was wearing a mask.
Now that I think about it, I found myself in the ER twice over the past year -- once in Columbus, OH, and the other in Philly. No one was masking so I had to find the courage to ask over and over. To lend some weight to my request, I made up some bs excuse each time, but everyone did it and almost everyone was pleasant enough.
These are great recommendations and a thorough list. I wanted ro cover a topic like this, but I think you nailed it and I’ll be referring others to this post. Thank you!