"It's Just Anxiety"... Or Perhaps They've Misdiagnosed You
Patients with POTS are frequently misdiagnosed as anxious. An exploration of the diagnostic process, the gaslighting and barriers patients face when dealing with this debilitating condition.
This is the second post in my series about POTS and Dysautonomia - a condition that has drastically altered my life. POTS stands for Postural Orthostatic Tachycardia Syndrome - and is one of a number of conditions that fall under the broader umbrella term of Dysautonomia.
What IS Dysautonomia? It’s a malfunctioning autonomic nervous system. That’s the part of your brain responsible for all unconscious processes. Anything you don’t have to think about - that your body is meant to do naturally - may go haywire. Heart rate, blood pressure, temperature, respirations, digestion - these things are all regulated by the autonomic nervous system. If you missed Part One in the series you can read it below:
As you can imagine - given how critical this system is to the functioning of our bodies - when it doesn’t work right it can manifest in a thousand different ways. Many of the early symptoms can look an awful lot like ‘anxiety’. High heart rate, dizziness, sweating, breathing too quickly - these things resemble a panic attack.
In fact - most POTS patients are misdiagnosed with ‘anxiety’ at some point in their diagnostic journey - often more than once. It can take years before you receive a correct diagnosis - and during that time we are gaslit, dismissed, profiled and unfairly judged.
It’s ‘JUST’ Anxiety - Or Is It?
I honestly can’t tell you when my POTS started. I was officially diagnosed in 2017 but had symptoms for a few years before that. During my twenties I battled Stage Four endometriosis - and because of the severe blood loss I was almost always hypotensive. When your blood pressure is low - your heart rate tends to be high. So - for better or worse - I learned from a young age to adapt to being tachycardic and dizzy.
I remember being in the ER back then - requiring IV fluids to prop up my dangerously low blood pressure. Doctors were stunned that I was even conscious with the vitals I had - and intrigued by what my heart did when I would stand up. They would bring med students in to watch the heart monitor and have me lay, sit and stand like a performing monkey.
At the time I didn’t think much of it - mainly because I was incredibly sick from the endometriosis. Being dizzy didn’t feel like a serious concern. If you haven’t read that story - you can read below:
After my hysterectomy I regained much of my lost health. The blood transfusions they had given me after surgery restored my hemoglobin to a healthy level - and I felt like Superwoman. Suddenly I could get out of bed, work and have a life.
I made the most of my newfound health - juggling two jobs, traveling, reviewing theatre and doing all the things I wasn’t able to do prior to my hysterectomy.
I enjoyed nearly ten years of relatively good health - and made the most of them. It was during that time that I become a theatre critic - a lifelong dream. I traveled to the UK and crossed a number of items off my bucket list. I still wasn’t as healthy as my peers - but compared to being bedridden from endometriosis - it was night and day.
Unfortunately my ‘good health’ didn’t last. I began noticing symptoms that were similar to what I felt when I was severely anemic - except my hemoglobin was completely normal.
I would sweat profusely while upright. I was exhausted ALL the time. My heart would race for no reason. I was no longer chained to a hospital bed - but my energy levels were noticeably different from my peers. I would spend weekends on the couch recovering from a busy week of work. I would decline invitations to review matinee theatre performances because I couldn’t get myself to the show for 2pm. I would get dizzy for no reason, had bad GI issues and intermittent chest pain.
Knowing this didn’t seem to be related to my endometriosis - I began seeing new doctors in an attempt to get answers. I wanted to figure out WHY I was still unwell. I wanted my new lease on life back. Their ‘answers’ left a lot to be desired:
You’re just anxious
You’re stressed
You’re working too much
You’re not working enough
Have you considered losing/gaining weight?
It’s just hormones (they used this one a LOT since hormones go wacky post hysterectomy)
Just don’t think about it
I don’t know
There’s nothing wrong
Your tests are NORMAL (this one is the bane of my existence as a chronically ill person. How often do we hear this? Doctors MUST learn to rely on more than just the most standard battery of tests which are often not indicative of how sick a person really is)
Finally I got to a specialist who believed me that something was indeed wrong. Her theory? Multiple Sclerosis.
I was terrified. I had lost most of my twenties battling endometriosis and I didn’t want to add a progressive life altering disease to my list of conditions.
She gave me a thorough work-up which came back negative for MS. Stumped - she too said it must be ‘anxiety’.
When you’re faced with a serious illness like Multiple Sclerosis - it can almost be a relief to be told it’s ‘just anxiety’ - but deep down I knew they were missing something.
Shortly after the specialist dismissed me with anxiety - I moved across the country for work and had to start over with a new team of doctors.
My new family doctor was wonderful and genuinely seemed to believe something was wrong - and she felt it was related to my heart. She referred me to a top cardiology clinic who gave me a battery of heart tests. Holter monitors, echocardiograms, ECGs etc. Once again I was told ‘your tests are normal’ and sent on my way.
I asked HOW everything could be normal when I had a racing heart on a regular basis? When I couldn’t stand up without the room spinning? When the chest pain was becoming more frequent and increasing in severity?
Image Description: A black and white photo of a girl laying in bed under a big white duvet. She’s cross legged and crouched forward holding her head in her hands.
They shrugged and said one of the most loathed lines in healthcare:
“What do you want ME to do about it?”
Doctors - stop saying this to patients. Our answer is simple and yet we’re often too polite to say it. We want you to do your job. We want you to get curious and dig a little deeper. To go beyond the most basic tests and think outside the box. We want you to NOT dismiss us as ‘anxious’ when we’re experiencing serious physical symptoms. We want you to FIGURE OUT WHAT’S WRONG.
Of course I didn’t say that - I simply shrugged and meekly said thank you. I walked away from yet another appointment with no answers beyond being told it was ‘all in my head’.
So How DID I Finally Get Diagnosed?
Honestly - it happened rather by accident. In 2016 I moved back across the country and landed downtown Toronto. Since I knew I didn’t have much energy - I found an apartment within a three block walk to work. This was the first time in my life that I would be walking to and from the office - having always driven in the past.
It’s three blocks right? How hard could it be? It turns out - very hard. Especially in the mornings. I would get up and do all my regular activities - hydrate and caffeinate and ready myself to face the day. I was exhausted - but that was nothing new.
I lived in a busy urban centre where thousands of people walked to work every day - many leaving from the same building as me. They were all energetic and walking SO fast. I couldn’t keep up - I shuffled along at a snail’s pace while watching everyone - young and old - pass me.
Half the time I would need to stop and sit on the pavement and get an Uber to come pick me up. Invariably it would take two to three tries to get someone to accept the fare because it was such a short distance. The driver would pick me up and point at my office building and ask my WHY I couldn’t just walk the rest of the way. I often had to promise huge tips just to get them to take me (one of my first experiences with the ‘crip tax’)
My illnesses were invisible - so other than being sweaty I looked fine. Why couldn’t I just walk the rest of the way? I didn’t have an answer - but I quickly grew tired of the question.
I saw more doctors who again told me nothing was wrong and that perhaps I was ‘out of shape’. I was NOT out of shape and could generally walk HOME from work without difficulty. I was practicing regular yoga, swimming and other cardio activities. Objectively I would be considered physically fit.
The medical system had no answers for me - so I continued to push myself to and from the office every day - often fainting en route and being terribly late for work.
One day - I passed out and became so disoriented that I couldn’t FIND my office. This was a route I took every single day and yet I couldn’t figure out how to get there. A kind stranger called 911 and they took me to the hospital where I was given IV fluids for low blood pressure but otherwise discharged with ‘nothing wrong’.
I was back in the ER a few weeks later - and that time they insisted I was hungover. I get it - POTS symptoms mimic a hangover - but I don’t drink. I’m terribly allergic to alcohol. They of course didn’t believe me and sent me on my way after effectively telling me I was a drunk.
Finally - I passed out in front of a number of friends and colleagues without any warning. I was fine and talking one minute - on the floor the next. Someone took me to the ER and helped advocate for me that this was NOT anxiety.
I’m forever grateful to that person. It had never occurred to me that I needed an advocate. I had been through so much health crap in my life that I considered myself adept at dealing with the medical system. I KNEW how to advocate for myself - so why would I need someone else?
It turns out I needed someone else to push past the ‘anxiety’ roadblock these doctors had. To make the patient blaming stop. To assure them I wasn’t a drunk. To tell them that I’m passing out suddenly and without any signs of fear, nervousness or anything else that would point towards anxiety.
It made all the difference. That ER doctor actually listened. They believed me that I wasn’t ‘fine.’ They gave me IV fluids to increase my blood pressure but rather than sending me home with no answers - they set me up with an urgent appointment in an outpatient clinic staffed by internal medicine doctors.
That appointment changed everything. I had a wonderful female physician who was deeply curious about what was happening to me. I spent almost eight hours at the clinic having a battery of tests done and being worked up by multiple physicians and nurses.
Their presumptive diagnosis? Dysautonomia. More specifically - Postural Orthostatic Tachycardia Syndrome or POTS.
They advised me to increase my salt and fluids and referred me to a cardiologist for further testing and to confirm the diagnosis. They may have saved my life. With how much I was fainting it was likely only a matter of time before I hit my head, fell into traffic or had another serious injury.
How is POTS Diagnosed/Confirmed?
POTS is in many ways a diagnosis of exclusion. Your doctor will run a number of tests on your heart to ensure that there’s nothing else that could be causing your symptoms. In the vast majority of POTS patients - the heart is structurally normal. There’s no underlying arrhythmia or congenital defects.
The issue is with the autonomic nervous system - which malfunctions and causes the heart to beat too fast. The goal of testing is to confirm you meet the diagnostic criteria for POTS while also ruling out other conditions that could be causing the postural tachycardia.
The diagnostic criteria is an increase in heart rate of thirty beats per minute (bpm) or more, or over 120 bpm within the first ten minutes of standing AND in the absence of orthostatic hypotension (OH is a different form of Dysautonomia - you can read more about it here). For children and adolescents the criteria is an increase of forty beats per minute.
How Do They Measure Your Standing Heart Rate?
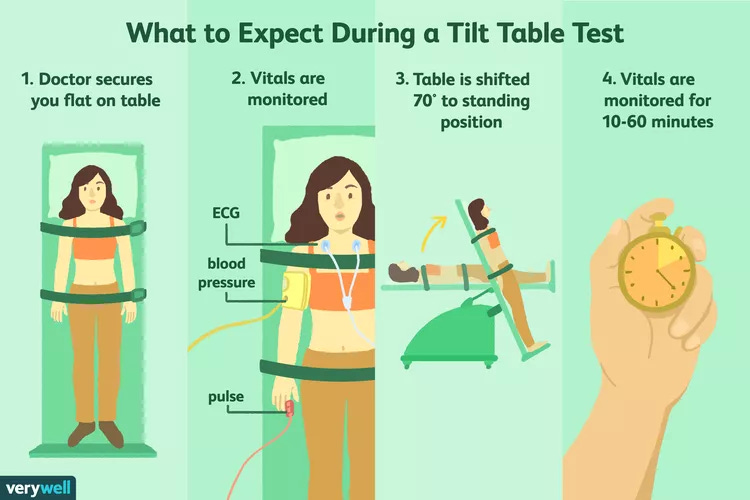
Generally speaking you will either do a NASA Lean Test or a Tilt Table Test. Both are accurate for the purposes of diagnosing POTS. The tilt table was considered the ‘gold standard’ test for years - but it is punishingly hard on the patient’s body and many doctors are opting for the gentler lean test instead.
For both tests - you will be asked to lay quietly in a dark room for 5-10 minutes to establish your baseline resting heart rate. You will be hooked up to an EKG to monitor heart rate and rhythm as well as have a blood pressure cuff to monitor your BP.
They will stand you up - and keep you standing for at least ten minutes. During this time you’re instructed not to shift your weight, move your legs and arms or talk. Effectively you can’t DO anything to encourage blood flow - they want you to stand completely still so they can observe whether your blood vessels can push blood back up to your heart and brain on their own (spoiler alert - mine can’t).
The Dreaded Tilt Table
Image Description: An infograph showing a women on a tilt table. 1. Doctor secures you flat on the table. 2. Vitals are monitored. 3. Table is shifted 70 degree to standing position. 4. Vitals are monitored for 10-60 min. Image Courtesy of VeryWell Health
When I did my tilt table test - I had NO idea just how much I shuffled my weight when I’m standing. Looking back it makes sense - when you move your legs or bounce up and down you’re encouraging the muscles to squeeze and pump blood back to your heart.
On a tilt table - your arms and legs are strapped down so it’s impossible to redistribute your weight in any way. Needless to say - I went downhill FAST. Within five minutes I was sweaty, nauseous and having blurred vision. Within seven I was throwing up and everything had greyed out. Within eight I was BEGGING them to stop.
They stopped the test before I fully lost consciousness because I was apparently screaming profanities at the staff - something which I’ve never done in my life. My brain was so deprived of oxygen that I don’t even remember doing it.
They put me in trendelenberg position (upside down) and pumped me full of IV fluids to calm my heart.
Needless to say - I received my POTS diagnosis after that test. I also spent WEEKS trying to recover my baseline. It put me into a huge flare. It was eye opening to realize just how much my lifestyle adjustments - most made unconsciously - were helping my condition.
Simple things like always having cold water on hand to chug if I became dizzy, squeezing and contracting my leg muscles and SITTING DOWN at the first sign of trouble had been keeping me from having more attacks. The tilt table effectively provoked the most severe reaction possible - and boy did I pay for it.
As a result - I tell patients who are already suffering from fatigue and energy limitations to talk to their doctor about whether the tilt table is TRULY necessary. If the NASA lean test can be substituted - it is easier on the body.
There may be circumstances where the Tilt Table IS necessary - so here are my tips and tricks to get you through:
Make sure you have someone to give you a ride home. Don’t rely on a taxi if at all possible - because you may be woozy and disoriented
Plan to take a few days ‘off’ from whatever your normal activities are to really rest and recover
Speak to your doctor in advance about what medications need to be discontinued. They often ask you to stop ALL medications but you have the right to say ‘no’ if you feel unsafe
I was instructed to fast for six hours prior to my test (this is to reduce the risk of aspiration if you vomit on the tilt table). My blood pressure runs incredibly low and without fluids the test was far worse. If I had to do it again I would ask to be permitted water or have IV fluids run in advance
Have compression stockings on hand for after the test. You can’t wear them during but you will likely appreciate them on the way home!
Make sure you’re stocked up on electrolytes and your favourite salty snacks so you can rehydrate after
Bring a change of clothes if you don’t plan on wearing the hospital gown - my clothes were soaked and smelly and I wish I had something else to wear
Rest, rest and then rest some more. The tilt table pushes your body to its absolute limits - there’s nothing to be gained from pushing it more in the days following. The more you can rest the faster you will recover
What Other Tests Can You Expect?
Generally speaking - since POTS is a diagnosis of exclusion - you will likely go through extensive cardiac testing to ensure there’s nothing else going on with your heart. Depending on where you live and whether there’s an autonomic lab - you may also have autonomic testing.
Here’s a list of the tests I had to confirm my POTS and rule out other cardiac and neurological diseases. I’m including my ‘top tips’ that I wish I had known BEFORE my first set of tests were run:
If you have MCAS I strongly recommend asking if you can use a barrier spray like Cavilon on your skin before the holter monitor
Technicians will often prep your skin with rubbing alcohol and sandpaper - this can increase your risk of allergic reaction to the leads. If possible speak to your doctor beforehand to see if this part can be skipped. I make sure to exfoliate in the shower the day before and avoid any lotion on my skin - and I’ve never had an issue with getting poor results
Some doctors have moved to a newer style holter which is a boomerang shaped pad that goes across your chest. Many MCAS patient report worse reactions with this style (myself included). You can speak with your medical team about alternatives
This test is fairly simple but does tend to interfere with your sleep. Having a blood pressure cuff go off every 30 minutes has a tendency to wake you up. I find that if I sleep with my arm propped on a pillow so it’s as still as possible - it reduces errors and the number of times the cuff squeezes
If at all possible make sure you have a friend or family member on hand to help if the cuff falls off. It’s incredibly difficult to get it back on yourself (especially if it inflates while it’s off your arm). I once had to go downstairs and ask building security to re-attach mine - I don’t recommend this approach!
If you have MCAS or chemical sensitivities - it’s worth asking your medical team to avoid spraying or cleaning the unit with anything that has a strong smell. I always react to the monitor. I’ve found putting saran wrap around the cuff once it’s on my arm helps contain the smell
This is a relatively easy test where you will lay in a dark room and have an ultrasound done of your heart to check for abnormalities. You will be instructed to do a number of breathing exercises throughout but it’s painless
For this test you will be placed on a treadmill while hooked up to EKG leads. Once you hit your target heart rate you will be instructed to quickly lay down for an echocardiogram
The test can be difficult on POTS and ME/CFS patients because of the exertion required. If you’re prone to PEM speak to your doctor about whether you HAVE to endure the entire test or if a smaller increase in heart rate would be sufficient. It’s not worth pushing your body and enduring a setback if you don’t absolutely have to
Make sure you have someone to drive you home, bring extra fluids and electrolytes and budget a few rest days to recover
This test requires you to collect all your urine over a 24 hour period. Top tip - if you have POTS and drink a lot of fluid - you will likely need more than one bucket. I’ve had lab staff push back on this and insist ‘no one needs more than one’ - now I get my doctor to write on the requisition to give me THREE containers
It’s critical you don’t miss any urine - so if you don’t have enough containers and have to run to the lab it could impact the test. Better to plan ahead
The urine needs to be kept in the fridge. If this grosses you out - I recommend getting a cooler and filling it with ice and keeping the bucket on it. You should also urinate into a SEPARATE container - put it into the fridge or cooler to bring the temperature down and THEN place it into the lab provided container. This ensures you’re not inadvertently changing the temperature in the lab container
Plan to be at home for the whole 24 hour period (so you don’t have to carry your pee bucket around with you) and you can ask the lab for a ‘hat’ for the toilet which can make collecting your specimen easier
Not everyone has this test - I’ve got structural abnormalities with my heart so every two years we do an MRI to get additional images
You need a low heart rate for this test - so if the MRI makes you nervous and/or your resting heart rate is high you may be given a sedative to take beforehand. Make sure you have someone to drive you home.
If you’re claustrophobic - my top tip is to close your eyes BEFORE they put you into the machine - and don’t open them until you’re out. My blood pressure is so low I can’t have sedation - and this has gotten me through many two hour long scans
Pick a song, a meditation or anything you can memorize. Say (or sing!) it to yourself during the scan. This will help distract your brain from the loud noises. It also helps me to know how much time is left. If it’s a 90 min scan then I will sing an entire musical cast recording in my head. With each song I know approximately how much longer until I’m freed from the tube!
Contrast dye is often used for this test. If you’re allergic or have MCAS - speak to your doctor about alternatives. I followed a pre-medication protocol for my first MRI but still had a severe allergic reaction. Now we do the test without contrast - and as long as my heart rate stays low the images have been good
This test can be a bit painful - so if you have MCAS that’s triggered by pain - speak to your team about pre-medication and whether it would be beneficial
The test involves putting electrodes into your muscles to test the nerve functionality (many POTS patients have neuropathy as well)
This test uses electrical currents to stimulate your body to produce sweat. The technician will then measure how much you sweat to see if your body responds with an appropriate amount
Ensure you’re well hydrated beforehand - and speak to your team about whether any medications need to be stopped in advance
Image Description: A bright red glowing heart is seen against a black background.
For additional information about tests and the diagnostic process - POTS UK has an excellent overview here.
If you’re a doctor or healthcare worker - Dysautonomia International has put together a list of the ten things doctors should know about POTS. Highly recommend reading and sharing with your co-workers. The more doctors who can recognize this condition - the better!
Now That You’re Diagnosed - What Are the Treatment Options?
Since this article is already really long - treatment options will be covered in Part Three - Learning to Live Horizontally! Make sure you’re subscribed so you don’t miss it - all articles are free and I would love to have you.
Part Three will also focus on the lifestyle and home modifications I’ve made to make life easier, reduce fainting spells and learn to adapt to my new reality as a POTSie. If there’s anything you want to see included - or any questions you want answered - feel free to drop a comment or send me a message.
In the end - it was a very long road to diagnosis. There were many twists and turns and far too many accusations of ‘anxiety.’ If you’re a healthcare worker reading this - I encourage you to remember this one key takeaway:
POTS can look a LOT like anxiety. Patients are often young and fit females and they present with symptoms such as sweating, nervousness and high heart rate. Don’t dismiss them as anxious without first making sure you haven’t missed this crucial diagnosis. Fainting CAN be dangerous - and when you tell a patient it’s ‘JUST anxiety’ - you encourage them to push through their very real physical symptoms. This can lead to a worsening of their overall condition and an increase in fainting spells. A quick stand test should easily differentiate between anxiety and possible POTS. Anxiety is NOT postural.
I’m glad I finally got my diagnosis - but I wish someone had said sorry. No one ever did. There was never any remorse expressed for telling me it was all in my head - or for gaslighting me for YEARS about my very real symptoms. Most of the doctors I saw simply acted like it never happened.
I understand that doctors are hesitant to ever say ‘sorry’ for fear of liability and legal issues - but please understand how much it means to your patient. When you get a diagnosis wrong - WE are the ones who suffer. Hearing that you feel bad that you missed it - or didn’t believe us - can restore some of our faith and trust in you. It’s a small gesture of humanity that can go a LONG way.
For all patients struggling with this condition - please know it DOES get better. You learn your triggers, you get better at mitigating and managing setbacks, and in time you become a strong advocate so you can fight for the care you both need and deserve.
It doesn’t happen overnight - but together we will keep raising awareness about invisible illness and disability and make it easier for ourselves and the generations who come after us.
Do you have POTS? How did you get diagnosed? How long did it take? If you’re currently trying to get a diagnosis - what barriers are you experiencing? Leave your comments below - I would love to hear from you!






I'm 63 years old. I was diagnosed less than 10 years ago when I ended up being referred to a cardiologist because of a pulmonary embolism. In reviewing my extensive medical issues he came to the conclusion. His explanation,testing and tratment has focused primarily on my low blood pressure. I have compression stockings and take salt tablets. How long did my POTS go undiagnosed? When I was in grade school (1960's) we would have annual "check ups" with the school nurse. I have never forgotten the embarrassment when she was trying to take my pulse/blood pressure and screamed at the rest of the kids to BE QUIET!! because she couldn't "find" it (and forever after I was labeled as "zombie", "vampire" "dead girl" by my classmates.) MY first memory of feinting was when I was 12, though my grandmother says it happened even earlier. In school, I was often accused of "faking" my various health complaints to get attention or to get out of class. In my 20's I began to believe I was crazy after being accused of being a hypochondriac so often. Every decade, it seems I got another diagnosis of something that previously didn't have a label. But Thanks to your series I'm realizing that many of them (GAD, Fibromyalgia?, GERD, Vertigo, Light Sensitivity, chronic dehydration) all fall under Dysautonomia. Something that no physician has ever mentioned to me to this day! And I'm wondering which Dr I should discuss this with to get my POTS diagnosis expanded so that ALL my specialists will "GET IT" 🙄 I'm glad that the science and medical community is finally STARTING to piece it all together. I pray that further research into identification and treatment is being done (sooner rather than later) and mass education of the medical community is rolled out so NO ONE ELSE has to go through the psychological trauma of missed diagnosis for as long as most of us have. I can't explain how emotional I am to finally have validation. I can't begin to thank you enough!!!
This one rings some bells.
Thanks for laying it all out for us. It's good to learn, and you make excellent and important points.
I don't have POTS or dysautonomia, but as an early fibromyalgia patient, I've had to deal with some of the same obstacles and issues in getting diagnosis and treatment. Thankfully, I've never had to do a tilt table. That sounds excruciating. I'm sorry for what you had to experience to get a diagnosis and be taken seriously. Personally, my heart would be fine, but with the fibro nerve pain I have to shift around a lot just so the pain levels don't build up too much in any one spot.
I wish society was better about invisible illness. I remember my sister had knee surgery when she was in high school. From the outside, she looked fine. But she was recovering from then-experimental surgery and couldn't put weight on her leg for any substantial period. And yet people would see what looked like a young healthy girl sitting on the bus and pressure her to give up her seat, with no idea of what was going on beneath the surface. That kind of thing happens way too much. "Why do you need a cab to go a couple of blocks?" "Why don't you give up your seat on the bus?" "Do you really need the elevator?" "Aren't you just being lazy?" It's all just ableism, and we need more education and awareness around invisible illnesses.
We also need people to be less afraid of taking the measures they need to protect themselves. I had so much pain and fatigue I could hardly walk. I memorized routes across the kitchen. Where are the handholds? Where can I push off to give myself a boost to get across the gap where there is nothing to hold on to? Where do I need to aim so I launch myself at a handhold without risking crashing into something? I did that for a couple of years before realizing that I really should be walking with a cane. I was in my 20s. I looked healthy from the outside. Wouldn't people judge me for using a cane? Wouldn't they think I was faking it, or looking for attention? You young fool. You need this. And no one cares that you're using it. And the fact that you are using it shows them that there's something going on, so most of them will actually be more understanding, not less. And the ones who do judge you for using an assistive device that you very much need? They're the ones who are lacking.
(Side note: My aunt invited me to have dinner at the clubhouse restaurant where she lived. I barely managed to walk across the room. Exhausted, tottering, leaning on my cane. My head was down the whole time because I could barely see straight. Woozy and short of breath, I collapsed into the chair and paused to rest. An elderly man got up from his table, walked up to me, and told me it was inappropriate for me to be wearing a hat indoors and I needed to take it off. I decided to bite my tongue for my aunt's sake. I didn't want to cause her problems with her neighbors. I was also still woozy and short of breath. I would have taken the hat off once I'd collected myself. But all I can think is... If that guy sees a disabled person wobbling across the room and decides that his top priority is to interrupt his meal so he can chide me for a minor breach of decorum.... I truly, from the bottom of my heart, pity him and the small bitter life he must lead. Besides, I started wearing hats everywhere because I lost my hair in elementary school and I was really sensitive about it. Even after I got used to being bald, with the fibromyalgia hypersensitivity, I very much needed the hat to protect my eyes from overwhelming light levels. It's also a disability aid in a way. But he never stopped to consider that I might have medical needs.)
But what I really appreciate is you calling out medical gaslighting. "It's just anxiety. It's all in your head. Push through it. Cope with it. Cope with whatever in your life is scaring you." No, no. It's that my immune system totally screwed up my nervous system and the tests you've run so far aren't able to show that. I get that doctors have to deal with a lot of patients who really are worried over nothing. And some things really do have simple minor fixes. But too often, doctors just dismiss patient concerns and real symptoms that really are a sign of something deeper going on that really does need to be addressed. They also suffer from tunnel vision. They know their speciality. They completely forget anything outside of it. They don't see the body as a whole. They forget how things interact. And... if the problem doesn't fall within what they're able to detect for their speciality, then they pass the buck. It's some other doctor's problem. Good luck to you.
I know how frustrating it is for doctors who truly want to help their patients, but who have to work within the limits of human capability and current technology. There's so much we don't know and so much we can't fix, for all the amazing improvements we've had over the last century. I have had many doctors tell me over the years that there's nothing more they can do, that they don't know how to help me, that they wished they could do more. I think knowing that my dad is a doctor helped them open up about that. I saw how much it hurt them to have dedicated their lives to learning how to heal people and then just being confronted with a problem they don't have the tools to address.
But too often they simply don't listen. They tell you it's all in your head. They see that the test results are normal, so instead of looking for another test, they gaslight you and dismiss you. When I was 16, my parents took me to CHOP (world-class pediatric specialty hospital in Philly) and the doctor listened to me and my parents and sent me home with two new medications. He took my parents aside to tell them about it. A few days into it, when it was clear it wasn't helping, Mom, wracked with guilt, tearfully confessed that they were placebos. He made her lie to me. Because he thought I was faking it and just needed something to believe in. Even though we'd only come to him after I'd been to a dozen other doctors and tried I don't even remember how many real medications.
The tests show normal, so it must be in your head. How many people have been actively harmed by that? Not just left untreated, but told to ignore their symptoms and their bodies' limits? And shamed for being ill? Infuriating.
I did have one doctor apologize to me once.
The first doctor to correctly diagnose my fibromyalgia. He was the one who developed the test that was used in the 90s (before it was replaced with better ones). He told me the good news. He knew what was happening and if I followed his protocols he guaranteed I'd be feeling better in a matter of months. I did everything he said. I didn't get better. He told me to my face I was lying. He said if I wasn't getting better it could only mean I wasn't doing what he'd ordered, and he couldn't treat a patient who wasn't honest with him. He screamed at me to get out and never come back.
A few years later, I did see him again. After he'd talked to my parents. (He knew them socially, since Dad was a professional colleague.) He sincerely apologized to me. He said he was wrong to do that, and he shouldn't have taken his frustration out on me, and he knew better. And he tried again to help me with what he'd learned in the intervening years.
But, for all the dozens and dozens of doctors I've seen... Neurologists, cardiologists, pediatricians, rheumatologists, sleep specialists, endocrinologists, and I don't even remember what else. Specialists. People in specialty hospitals. In half a dozen different states. Sometimes traveling hundreds of miles for an appointment. ... With all that, he was the only one who ever apologized for anything other than not being able to be more helpful.
He was not, however, the only one who yelled at me, who dismissed me, who accused me of lying or faking it. We traveled 300 miles to see a specialist in Boston, who listened to me lay out everything I'd been through and just ask for his help, and got mad at me, walked me down the hall to the cancer ward, showed me a patient of his who was dying of leukemia, and told me to leave and not come back until I had real problems. I saw an endocrinology researcher who said I don't have the genetic markers he'd identified, so clearly I couldn't be diabetic and if I'd just stop taking insulin my body would realize it needed to make its own. (Thankfully, I knew better than to listen to that claptrap.) I saw him again years later for something else, and he didn't apologize.
Medical science has limits. The tests can only show a limited amount of information, and you have to know what to look for. I get that doctors are pressured to find ways to help and sometimes they just can't. But they need to be honest with us. To step off the pedestal and work with us. Believe us. Listen to us. And say "I'll keep looking. We'll try something else. I'll talk it over with some people who may know more." I've had that happen a few times, and it's been encouraging. Refreshing. So much more helpful and supportive.
I really wish doctors were taught to work with patients instead of handing down judgements and decrees. I also wish they remembered that zebras do exist, even if they are rare and sometimes hard to spot.