Learning to Live Horizontally - Your Guide to All Things POTS
When you have POTS - being upright is a challenge. We deal with fatigue, tachycardia, dizziness, fainting and more. Adapting to living life horizontally can make symptoms more manageable.
Are you horizontal right now? Do you have your legs up the wall? Are you lying down? I am - because that’s what this entire article is about. Learning to live your life horizontally to cope with POTS/Dysautonomia and other energy limiting conditions like Long Covid and ME/CFS.
This is the third and final article in the series about POTS which kicked off Dysautonomia Awareness Month. If you missed the first article - you can read it below:
When you’re living with POTS - gravity is NOT your friend. Our bodies do not function properly when upright. As a result - most of us feel our best when we’re horizontal.
Unfortunately - the world is not designed for people who need to be horizontal. We live in a vertical society! Adaptation is key - and it can be a long and hard road.
This article will explore treatment options and lifestyle modifications to make life as a POTSie a little bit easier. If you’re new to this condition and feeling frustrated and scared - please know it DOES get better. There may not be a cure - but there are lots of things you can do to increase quality of life and decrease symptoms.
This will be a long one that leaves no stone unturned - so settle in, get cozy and let’s look at how to be the most comfortable POTSie you can be!
The first two sections will deal with the most common supplements, salt and pharmacological interventions.
If you’re already doing those things and came here looking for lifestyle tips and home adaptations to manage living horizontally - you can skip down to Part Three “Living Life Upside Down”.

Image Description: A woman with red hair and a pink dress lies with one arm outstretched on the floor.
You’re Diagnosed with POTS - What Comes Next?
First things first - it’s great that you’ve been able to get a diagnosis. POTS is still poorly understood and recognized - and there are significant barriers to obtaining diagnosis and treatment.
If you’re still without diagnosis - please read my second article in this series which is dedicated to the diagnostic process:
Once you’re diagnosed - many doctors will start you on a regimen of increased fluids and salt intake and advise you to use compression stockings.
This is the most conservative and non pharmacological approach. POTS patients are often hypovolemic - meaning they have low blood volume in their body. Increasing oral intake of salt and fluids can help offset this - and compression stockings assist in pushing blood back up to your head from your legs.
Doctors will hopefully advise how much salt to consume - and I recommend getting it in a tablet or liquid form so you can be sure that you’re hitting your target. It’s incredible just HOW much salt many of us need to consume to reduce symptoms. Getting it through diet alone is a huge challenge. Dysautonomia International has a great overview of salt versus sodium - and how much to aim for - here.
If you want to get it through diet - try to measure out your salt requirements in a small dish and make sure it’s empty at the end of each day. Personally I couldn’t stomach the taste of my food with that much salt - so I take Vitassium salt tablets and Nuun oral rehydration solutions.
Other good options are:
Pedialyte
Gatorade (ideally low sugar options)
Liquid IV
LMNT
Normalyte
You can also get plain salt tablets from any pharmacy - though most patients report they’re hard on the stomach. The benefit of a tablet like Vitassium is that it’s designed to reduce irritation in the GI tract.
If you have the energy and spoons - you can DIY your own solution as well. Some patients even make their own capsules at home for considerably less money than the store bought options. You just need to find the right amount of sodium and potassium, buy the raw ingredients in bulk and add them to empty pill capsules.
It’s important to note that sodium and potassium are critical minerals - they work together in the body. If you get too much of one - it can negatively impact the other. Ideally your doctor will run a 24 hour urine sodium test as well as blood tests for sodium and potassium to ensure you’re staying in the correct range. Tips for the 24 hour urine test can be found in Part Two of my POTS Series.
Compression stockings are the other thing that the vast majority of POTS patients try right away. These are medical garments specifically designed to help squeeze blood back up from your legs to your heart and brain.
You can get them in various ‘strengths’ which refer to how tight they’re going to be - as well as various sizes such as knee length, thigh highs and ones that go all the way to your waist like panty hose. You can even get abdominal binders if you find you have blood pooling in your abdomen.
I’m going to be honest with you - they can be quite uncomfortable and do take some getting used to. If you have comorbids like MCAS or EDS - you may have additional struggles. My MCAS is triggered by anything tight on my body - and my vEDS means I bruise VERY easily. As a result I found compression to be exceedingly painful and I only use it for particularly difficult circumstances (flying, after a tilt table test etc).
If this is your first time wearing compression stockings - try and have someone on hand to help you and/or ensure you are well rested before you try and put them on. They take a surprising amount of energy to get up one’s legs.
My top tip - and one I wish I had learned earlier - is to put them on in bed first thing in the morning before gravity gets the better of you. When I wake up I drink 1L of water right away - do a few ankle pumps and calf raises and then put the compression socks on.
If I wait until I’ve gotten up and had breakfast or taken a shower - my lower leg swelling is so severe that it’s double the effort to put them on. I’ve passed out with one leg on and one leg off - I don’t recommend it!
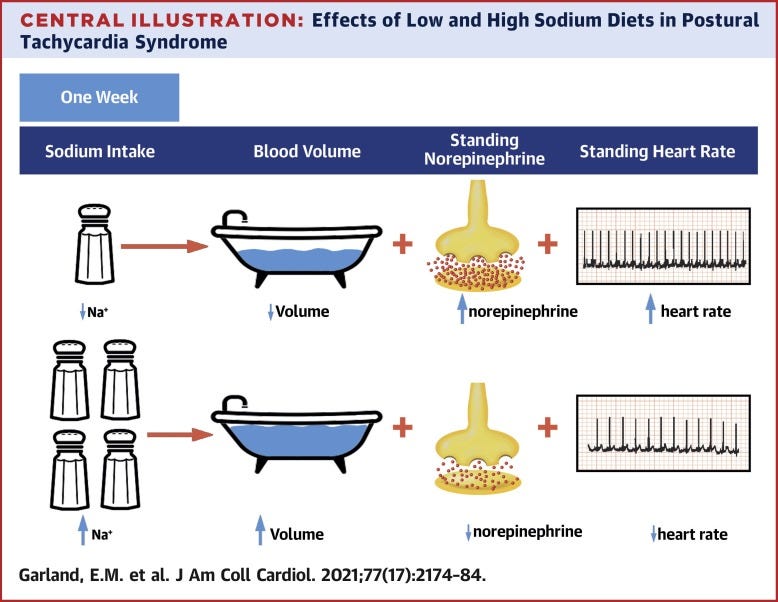
Image Description: A flow chart showing the impact of increased salt intake on blood volume, standing norepinephrine and standing heart rate. Image courtesy of Normalyte.
What About Medication Options?
Now that we’ve tackled salt and compression - it’s time to look at the various medication options that exist for POTS patients.
Full disclosure - this is NOT medical advice. Every medication has a risk and benefit analysis that you need to review with your doctor. This will be extra complex if you’re also dealing with MCAS. Due to various comorbids I have - most medications for POTS have not been an option for me - but I will still go through the most common treatments for those who may benefit from them.
These medications act by lowering your heart rate and causing it to beat with less force. For people who’s primary issue is intense tachycardia - they can be a great option but are contraindicated in those with low blood pressure (like me!)
This medication is a corticosteroid that acts on the kidneys to increase salt reabsorption and potassium excretion
Because it causes your body to retain salt - it has the potential to throw off your potassium. Potassium is crucial for proper heart function and therefore it’s recommended you have your blood levels monitored regularly when taking Fludro
It can also cause weight gain - so if this is a concern and/or you also have EDS - it’s worth discussing with your doctor ways to manage weight while on this medication
This medication works by causing blood vessels to tighten - thereby increasing blood pressure and sending more blood back to the heart and brain
Supine hypertension is a risk with Midodrine - so most patients are advised not to lay down for 4-6 hours after taking it. If you have ME/CFS and/or severe PEM - it may not be a good option
This medication works by slowing your heart rate without impacting other cardiac ionic currents
It can be prohibitively expensive though a generic version was recently approved in the US
IV Fluids
Giving IV fluids is generally only considered when all other medications have failed (due to its invasive nature). IV fluids increase your blood volume and pressure and lower your heart rate
Many POTS patients report feeling tremendous improvement on IV fluids - but the risks have to be carefully weighed against the benefits
If using a peripheral IV - you will eventually lose access as repeated poking is hard on the veins (this may happen faster if dealing with EDS)
When you no longer have peripheral access - you will need to consider a central line such as a PICC or a Port. These allow you to administer IV fluids yourself at home - but they carry a significant risk of infection that can become life threatening sepsis
Those are the most common medication interventions for POTS - for more information check out POTS UK who have a comprehensive and easy to read medication and treatment overview.
Living Life Upside Down
We’ve tackled all the most common POTS interventions that doctors are likely to suggest - but what can you do on your own? What kinds of tools can you leverage to make life as a POTSie more bearable?
This is where I’ve put the bulk of my very limited energy - adapting my home and lifestyle to accommodate my need to be horizontal.
Due to my unique comorbids and dangerously low blood pressure - I was ineligible for most pharmaceutical interventions. I had to get creative and think outside the box.
Most of the things I do I learned the hard way through painful trial and error - so my hope is by sharing them with others they might be able to avoid some of the pain and injuries I’ve sustained over the years.
We’re already horizontal - so let’s dive in (this will be a long one - feel free to take breaks)
First things first - you need to ‘POTS Proof’ your home. It’s similar to baby proofing - you want to carefully assess the various parts of your living environment for dangerous corners, edges and other things that could hurt you if you faint or fall down.
I’m going to go through each room in my home and give the tips and tricks that helped me be a bit safer.
I live in a small condo. It’s approximately 500 square feet with no stairs or carpets which reduces the tripping hazards. While it can be difficult to be confined to such a small space - it’s also beneficial in that I never have to walk far to get to what I need. The bathroom, kitchen and bedroom are all within about ten paces of my bed. Not everyone enjoys tiny living - so I will try and include tips for homes of all sizes!
Bedroom:
Elevate the head of your bed. Many people think they should elevate their feet because that’s what helps POTS patients during the day. However when sleeping it’s more beneficial to elevate your head. You can do this with a bed wedge or by putting the top of your mattress on bricks or books. Sleeping this way helps improve morning orthostatic intolerance
Make sure your bed is comfy! POTS patients often experience a lot of pain due to their muscles contracting so hard to push blood back to the brain. A cozy bed can help
Have extra pillows and a soft headboard that you can put your legs up on. Being able to put your legs ‘up the wall’ can help tremendously when tachycardic. I make sure my bed is set up so I can flip around any time I need to
If you wake up in the middle of the night with tachycardia - consider keeping an ice pack in bed. I’ve found that if I wrap an ice pack in a towel it stays relatively cold - and when I wake up I can immediately place it on the back of my neck for relief
Try a white noise machine and/or an air purifier. I have both and they’ve helped tremendously. In POTS our nervous systems are dysregulated - so being woken up by sudden noises can trigger an attack. I use white noise and earplugs to reduce those sudden wake ups. The air purifier has improved the quality of my sleep and reduces mast cell triggers which can drive a POTS flare
Get a pregnancy pillow! I’m unable to have children - so the idea of using a pregnancy pillow felt strange to me. Once I got one - I wished I had done it sooner! We need one aimed at people with chronic illness. You can shape it into a ton of different positions that can help with pain, tachycardia, leg/head elevation and more. Highly recommend. Plus they’re cozy.
Image Description: Kelly laying on a white bed with a grey pregnancy pillow. She’s wearing grey sweatpants and slippers and a beige sweater.
Bathroom:
The bathroom is one of the most dangerous rooms in the house for a POTS patient. Both showering and using the toilet can trigger a vagal response and lead to fainting
Get a shower stool/chair. I resisted this for a LONG time because I felt like it was ‘lazy’. I wish I had been kinder to myself. Fainting in the shower is dangerous and even if you don’t faint - showering takes an absurd amount of energy (or ‘spoons’) and much of that can be alleviated with a chair
If you’re able (I can’t because I rent) have hand railings installed in your shower. Having something to grab onto when you feel faint is a big help
Avoid baths and/or make sure you have someone to help you when you stand up after a bath. Laying in warm water for an extended time will dilate your blood vessels and increase odds of dizziness and fainting
Make sure you have a non-slip bath mat. You could also get shower shoes to reduce odds of slipping. I use Crocs and find they help my feet have something to ‘grip’ which reduces the dizziness
Check the height of your toilet. If you can access an occupational therapist they can assess your gait and height to help you determine how high your seat should be. Mine suggested I raise my seat one inch (you can buy a riser to do this) and I thought it was the silliest suggestion. How could that make a difference? Turns out - it helps tremendously. Not having to squat so low makes getting on and off the toilet safer
Consider a squatty potty! If you don’t know what these are - check them out. They can make bowel movements easier which saves energy and reduces odds of vasovagal reaction
Kitchen:
I would argue this is the second most dangerous room in the house (after the bathroom) Fainting while cooking is something that needs to be avoided at all costs
If you can get a counter height stool to sit on while doing food prep or clean up - you can save a lot of energy
Anti-fatigue mats can help as well
I wear thick nitrile gloves. These serve two purposes - they prevent skin tearing and infection since my EDS causes thin skin - but they’ve also helped me avoid some cuts and minor burns by serving as a protective layer
Use the microwave whenever you can - it may be your best friend. The stove and oven put off heat and heat can trigger a POTS flare
Have a glass of ice cold water nearby at all times. Chugging cold water can temporarily stave off a faint
Have an icepack readily accessible. Putting it on the back of the neck can reduce heart rate quickly and buy you time to turn off stove or oven
Sing! Or talk loudly to yourself. It’s helped me buy myself a few minutes to get safely to the ground
If cooking alone - have a ‘safety buddy’. I once passed out with the oven door open and woke up with pieces of roasted sweet potatoes all over me and a VERY hot apartment. Now I make sure to text a friend when I’m cooking and have them call for help if I’m non-responsive after a certain length of time
Living Room/Office:
People often ask me how I write with POTS. Before I became severe I had an office chair that was big enough for for me to sit cross legged. Having my legs elevated in that manner made it easier to sit upright for long periods of time
I also used to sit on a Yoga ball. They engage your leg and core muscles and can help increase blood flow to the brain
If you’re able to work on a chaise lounge or a recliner - those are great options as well
If in an office environment see if you can have a second chair or a stool to place under your desk to elevate your legs
Bolsters are helpful. I do all my writing horizontally now - and I use yoga style bolsters to elevate feet and legs
Having a light phone and laptop make this much easier. I have an iPhone mini and a Macbook mini and both are small enough to rest comfortably on my stomach when I need to be fully inverted. I also find a lighter phone fatigues me less when I have to hold it upright
Other Helpful Home Tips:
Water bottles are your friend! Keep them stashed in various parts of your home so that if you suddenly feel woozy you can easily access something to drink
Keep chairs or stools handy in places you know you might get faint
Cover all sharp edges and remove things that could be dangerous during a fall
Consider replacing glass dishes with plastic ones (if your MCAS can tolerate it). There’s nothing worse than fainting on broken glass
If you have stairs - make sure to have a handrail to use when going up/down. If you don’t have a hand rail see if you can get one installed. Failing that - you can always go down on your butt!
Have salty snacks on hand! MCAS can make this a challenge - but before my MCAS became severe many of my go-tos were things like pickles, sauerkraut, olives, pretzels and sometimes potato chips. I would aim for low carb and high sodium snacks whenever possible
This one is a bit silly - but many of us spend a LOT of time on the bathroom floor. It’s understandable - POTS can cause GI issues and the bathroom is a place we’re prone to faint. Make your bathroom a happy place! I put sunflower decals on the lower half of my wall so when I’m stuck on the floor it feels like I’m in a garden. It’s just one small way I’ve made the experience a tiny bit easier and more comfortable
What About Ways to Work, Socialize, Exercise etc?
We’ve gone over the various ways you can set up your home to make living with POTS easier - but what about when you’re not at home? How can you exist in public safely, effectively manage your energy levels and lessen the odds of a flare up?
Managing Energy Levels:
People with POTS get fatigued very easily. Our muscles are constantly working overtime to try and push blood back to the brain. Compression stockings can help a lot - but pacing is also important. My best tips for managing energy levels:
Learn your average resting heart rate. Once you know this - you can monitor and see when it’s going too high
Everyone with POTS has a different threshold for ‘too high’ - you have to experiment to find yours. When mine gets too high I immediately stop my activity and get horizontal if at all possible. I find this helps avoid some of the crushing fatigue that comes from unrelenting tachycardia
Do NOT be afraid to rest. Your heart is effectively running a marathon any time you’re upright - it’s OK to be tired. Give yourself the permission you need to put your legs up and take a break. Pushing through tends to make things worse
Hydrate. Especially if you know you have to physically exert - make sure to consume extra salt and fluids ahead of time and during exertion
Consider eating low carbohydrate meals more frequently. Large meals high in carbohydrates require a lot of energy for digestion and can leave you tachycardic and exhausted. Meals higher in fat and protein and eaten more frequently throughout the day can help
Avoid alcohol. I know many people don’t want to hear this - but alcohol is dehydrating and almost always worsens the symptoms of POTS
Some people also need to avoid caffeine - though in others it can actually help. My blood pressure is so low that caffeine actually REDUCES my heart rate by temporarily increasing blood pressure
Being Out in Public
It can be scary being in public when you’re prone to fainting or dizziness spells - thankfully there are ways to make it easier:
Always carry water and electrolytes. I can’t tell you how many times I was able to buy myself a few more minutes to find somewhere to sit by chugging salty water
Wear a medical alert bracelet and/or ensure you have documentation about your condition on you at all times. I’ve been harassed for sitting on the floor of various public places - and having documentation that shows it’s a disability accommodation has been helpful
A medical alert bracelet will also help if you lose consciousness in public. It’s important for first responders to know the likely reason you passed out
Don’t be afraid to look silly. I know this can be hard - but try not to care what other people think. I’ve sat (or laid) down in the strangest of places. My goal is always to get to the ground as fast as possible and in the safest place (you don’t want to be trampled). If this means people stare at me? Let them stare
The ground in public places can be dirty - consider carrying a dropcloth and/or something like a raincoat with you to put on the floor. I always had something I could easily wipe/wash in my bag - and would place it down before sitting
Have a clean change of clothes at your front door. Sometimes I was forced to lay down in some particularly dirty places. I’ve had to lay on the floor of a crowded ER or a shopping mall during busy sales. When that happens I come home and immediately change and wash clothing
Have all your medications on you as well as a list of medications you take. Should you end up needing the hospital - you will be glad to have it
Be aware of your surroundings. I remember one of my doctors saying to me ‘POTS won’t kill you - but fainting in front of oncoming traffic could.’ It felt dark at the time - but they weren’t wrong. Try not to stand anywhere that could result in immediate danger should you pass out
Lines are NOT your friend. Walking is generally easier for POTS patients than standing still. If you’re caught in a long line - try and shuffle your weight from side to side. I used to do standing yoga poses (remember what I said about not caring if people stare?) and they almost always prevented me from passing out
Consider whether it’s safe for you to drive. I no longer drive as I pass out too frequently - but the decision of whether or not you can drive is between you and your doctor. If you ever become woozy behind the wheel - pull over as soon as possible and elevate your legs. Keep electrolytes in your vehicle at all times
Mobility aids are your friend - especially where long lines are concerned. More on that in the next section
Avoiding Deconditioning
When you’re diagnosed with POTS - you will likely hear a LOT about deconditioning. You may even be told it’s the reason you developed POTS (something which has been thoroughly debunked). It can be easy to push your body to exercise more so that you can stave off worsening symptoms - but pushing often leads to setbacks and flares.
It’s important to find safe and effective ways to strengthen your leg muscles while working within the limits of life as a POTSie:
Recumbent exercises are generally the best tolerated. Things like a stationary bike, a rowing machine or even arm bicycles to strengthen the upper body. Treadmills and ellipticals are much harder for us
Swimming is another fantastic option if you can tolerate it (many of us with MCAS are allergic to the chlorine). Make sure you don’t swim alone in case you get fatigued and/or faint
There are exercises you can do in bed to strengthen your legs and help move fluid out of your lower body. I do these whenever I’m able - Bob and Brad are absolutely hilarious and following their routine makes me smile:
You can look into a cardiac rehab program - some hospitals offer these as a safe place to exercise with medical supervision. There may also be programs aimed at senior citizens that could accommodate the need to be recumbent
Always keep an eye on your heart rate and listen to your body. If your heart rate is too high - or you feel woozy and dizzy - stop and rest. There is no benefit to pushing your body into a flare or a fainting spell - and there’s many safe ways to exercise when you’re ready and able
Mobility Aids:
Mobility aids can be a lifeline to people dealing with POTS - yet we are often hesitant to adopt them. Fears of being judged, questions like ‘am I disabled enough?’ as well as concerns over further deconditioning can all be impediments to getting the aids we need.

Image Description: A photo of a metal wheelchair with blue accents
I’m here to encourage you NOT to delay getting a device that could make the world more accessible (and safer). You would be surprised at how much energy you can save by using an assistive device.
I’ve been completely housebound for years - but before I became this severe I took a bucket list trip to the UK and Scotland. I agonized over asking for wheelchair service at the airport - and finally did it because I didn’t want to be so wrecked from traveling that I couldn’t enjoy my trip.
What a difference it made! It was the first time in years I didn’t need to spend 2-3 days recovering after a flight. Saving those spoons proved crucial to enjoying my vacation.
Wheelchairs aren’t the only options either - you can look into walkers, canes, or any type of device that might make it easier to stand and move around. I had a walker with a folding seat that I could open at any time if I suddenly needed to sit down. It was a game changer when I found myself stuck in a long line or on public transit with no seats.
Talk to your doctor, physical therapist or occupational therapist about what options might make the most sense for you. Speak with other patients - many have been dealing with these conditions for a long time and have found hacks and aids that could be life changing for you.
The struggle to adopt a mobility aid is very real - so I’ve included four articles below from fellow disabled writers who’ve spoken of their journey to accessibility and accommodation:
What Did I Miss?
I’ve been dealing with POTS since 2017 - likely long before that. I think I’ve covered most of the common pitfalls and struggles - but we are all wonderfully unique and have our own challenges.
If I missed something you want to see covered in a future article - please leave it in the comments section. Likewise if you’ve found a tip or trick that has helped you learn to live life horizontally - please share so other patients can benefit from your experience.
Wherever you’re at in your POTS journey - please know it does get better. While there’s no cure - there are a variety of treatments and lifestyle modifications that can reduce the severity of symptoms and improve quality of life.
It can be incredibly frustrating having to do so much trial and error - but I promise - when you find what works for you it will all be worth it.
Until then - let’s keep raising awareness about this condition in the hopes that better treatments come along. We may not be able to be vertical - but that doesn’t mean we can’t contribute, help others in their journey and lead full and happy lives.









Just wanted to mention that there is also subtype of POTS that folks often misunderstand called Hyperadrenergic POTS. I like to tell folks to think of POTS as a spectrum instead associating it strictly with fainting and remaining horizontal. Many POTSies are like you, some are hyper-POTS, others flip-flop between hyper and hypo trying to find a balance.
Omg, these articles are SO helpful! I figured out several months ago that there's a name and a whole explanation to the shit I've been experiencing, and ever since then I've looked up stuff online and read stuff here and there but haven't been able to find anything even close to this. Which is what I've been looking for: someone who has POTS and can write about it in detail. Not only can you do that, but alllll the damn info and suggestions you have are fabulous. I'm not diagnosed but I know I've had POTS since I was a kid. And it hasn't gotten any better.
Also, I'm constantly craving salt. This has been going on for so long and nobody has told me it's related to POTS. They didn't even mention POTS.
I could easily write an entire novel about how seen I feel in these articles and how much value I find in them. I'm SO grateful. I have a Resources post that I update whenever I find stuff that can help other autistic people. Can I add you to the list as someone very knowledgeable in POTS and disability so other people can find your stuff?
Thank you, thank you, thank you ❤️