Living Life Upside Down - An Intro to POTS and Dysautonomia
I live my life horizontally thanks to a condition called POTS (Postural Orthostatic Tachycardia Syndrome). It's poorly understood, often misdiagnosed and can be devastating to quality of life.
Are you lying down for this?
I am … because that’s how I live most of my life. Horizontal. Often upside down. I’m not an acrobat or a gymnast - I have POTS (Postural Orthostatic Tachycardia Syndrome). It’s a form of Dysautonomia - a literal malfunction of the autonomic nervous system. My body does NOT get along with gravity. It ceases to function when upright.
It took years to get a diagnosis. Countless ER trips and specialist appointments - most of whom told me I was fine and simply ‘anxious’ and/or that there was absolutely nothing wrong.
I didn’t know WHAT was wrong - but I knew there was ‘something’. I woke up every morning feeling dreadfully hungover - despite never consuming alcohol. I was dizzy, nauseous and sweaty as soon as I got out of bed. I would faint on my way to the bathroom, faint at work, faint in the supermarket. I frequently sat on the floor of public transit to avoid passing out on a stranger. I was exhausted 24/7 and spent weekends in bed trying to rest up and recover from a week of pushing my body through crushing fatigue.
When I FINALLY received a diagnosis in my thirties - everything started to make sense. All the strange and seemingly unrelated symptoms I had experienced were explained by this one beast of a condition. It WASN’T in my head. I WASN’T anxious. I WASN’T ‘fine.’
Getting a diagnosis changed my life - it opened the door to treatment options, lifestyle modifications and other ways to lessen symptoms. I want to take that knowledge and help educate patients on how to manage this condition.
I hope to bring more awareness to healthcare workers about the unique challenges a POTS patient experiences - as well as the pitfalls and roadblocks in obtaining a diagnosis.
This will be a three part series similar to the one I did on MCAS (Mast Cell Activation Syndrome). If you missed that one - you can check out Part One here:
This post is an introduction to POTS - I hope it will serve as an easy to digest welcome guide to living with this challenging condition. Part Two will be ‘Maybe It’s Anxiety - Maybe You’ve Been Misdiagnosed’ and will focus on the LONG road to diagnosis and the gaslighting that occurs along the way. Part Three will be ‘Learning to Live Horizontally’ and will be a deep dive into accommodations, tips and tricks to help manage Dysautonomia and the importance of knowing your baseline (and how this condition can impact all aspects of medical care).
If you’re not already subscribed - you can sign up for free below to ensure you don’t miss this series!
Living Life Upside Down - The Wild World of POTS
Image Description: A photo of Kelly laying upside down in bed with her legs up the wall. She’s on white bedding wearing grey sweatpants and big cozy grey socks. To her left is a blue pillow with a yoga image on it, to her right is a white pillow that says ‘Wild at Heart’. Her wall is blue and adorned with silver butterflies.
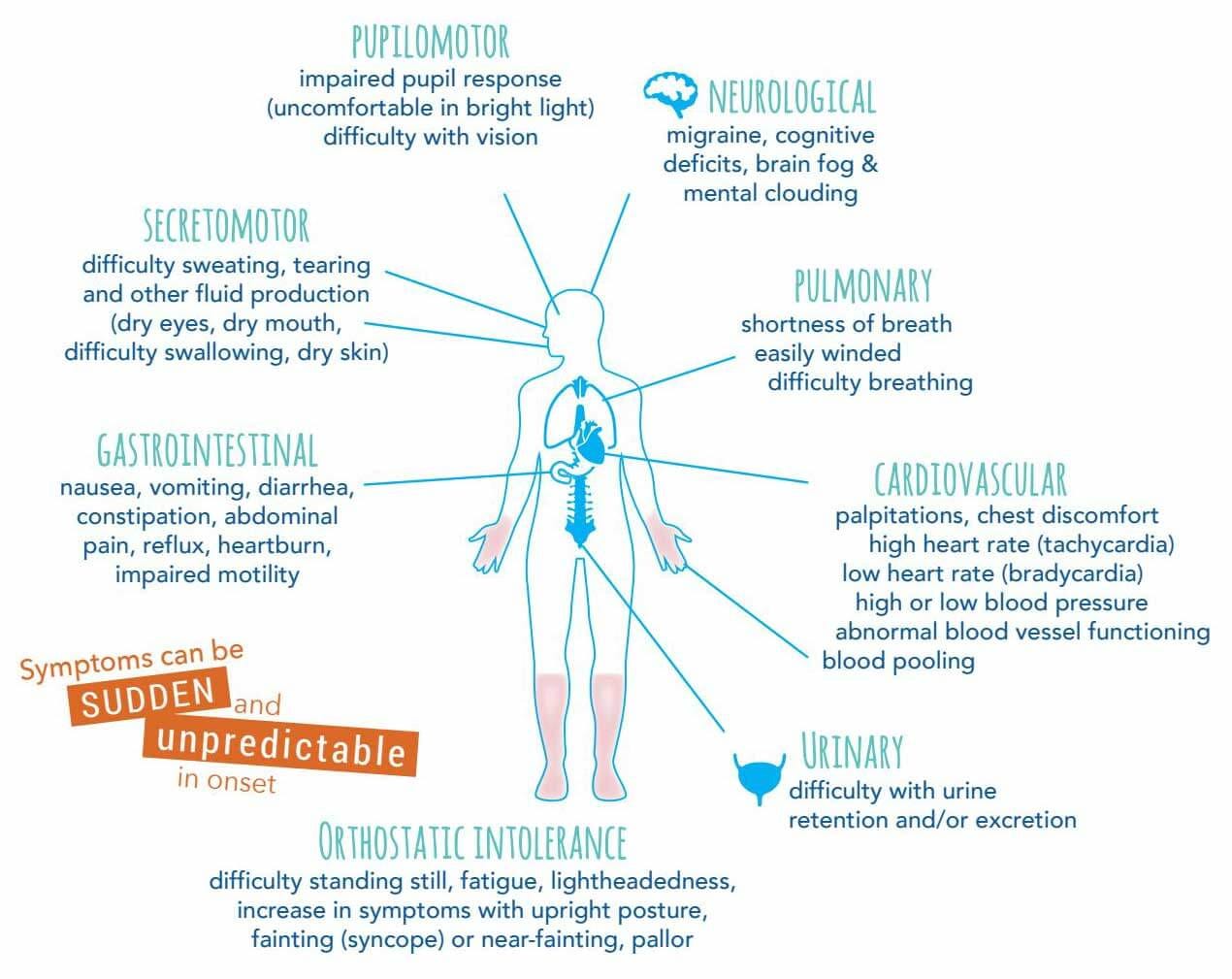
POTS isn’t just tachycardia when standing. Nor is it only fainting. Dysautonomia can impact nearly every system in your body. It is a malfunction of the autonomic nervous system - which is the system that controls unconscious processes.
That means everything from blood pressure to heart rate, respirations, digestion and temperature regulation stop functioning correctly.
A healthy person’s body will naturally regulate these systems without any effort from the individual. In dysautonomia they malfunction. One of the most noticeable ways this presents is with tachycardia when standing which can cause fainting - but it can cause so much more than that. You can have issues with low body temperature and/or fevers, severe gastrointestinal issues, your eyes can fail to dilate properly in the light (this one took YEARS for me to figure out), you may sweat too much or not at all. There’s virtually no part of the body that can’t be impacted by Dysautonomia.
When You Stand Up - What Happens?
In a healthy person - the moment you stand up your vascular system pumps blood back up from your legs towards your heart and brain. This happens unconsciously - you never need to think about it.
Close your eyes and picture yourself first thing in the morning. You wake up groggy from a good nights sleep and get out of bed. Do you think to yourself ‘hey blood vessels - can you send some blood to my brain now?’ Of course not. It just happens.
Unless you have POTS. My mornings look very different than a non-POTSie. When I stand up - everything starts to spin. My vision blurs out. My head and heart start to pound and I get sweaty and nauseous. If I don’t immediately sit or lay back down - I faint.
As a result I’ve had to train myself to remember to drink a huge glass of water before attempting to get out of bed. I do ankle pumps and calf raises to get the blood flowing and I stand up extremely slowly. Other people don’t have to think about this process - I have to concentrate with all my might on contracting my leg muscles to try and get them to FORCE blood back up to my brain. I’m effectively attempting to get my muscles to do what my blood vessels won’t do.
This is why laying with the legs up the wall is so effective - you’re changing the effects of gravity on your body. Your vascular system AND your muscles get a much needed break and your brain gets more oxygen.
POTS is More than JUST Fainting
As I mentioned above - POTS can and does impact all the systems of your body. I get terrible nausea, vomiting and diarrhea. I’ve developed swallowing issues. My eyes inability to dilate means I’m incredibly sensitive to light and have to wear sunglasses even on cloudy days. My blood pressure is so low that I experience confusion, slurred speech and impaired vision. I’ve experienced hypothermia as well as terrible fevers in the absence of infection.
It causes debilitating fatigue and terrible ‘hangovers’. For years I would wake up with a pounding headache, noise sensitivity, nausea and vomiting. It was exactly what hungover friends experienced - only I never consumed alcohol. My POTS causes me to dehydrate overnight and makes EVERY morning a hangover morning.
I find that people are generally incapable of understanding the depths of fatigue POTS patients have to cope with.
Imagine running a marathon - or doing any intense cardio. The goal when you exercise is generally to get your heart rate into target ‘fat burning zone’ right? When that happens you sweat more, you may get short of breath, your muscles burn and that’s how you KNOW you’re getting a good workout. You’re exhausted when it’s over - but it’s the good exhaustion that comes from knowing you accomplished your goal.
Now imagine your heart being in the target zone when you’re brushing your teeth. How about when you sit up in bed? Or when you need to take a shower? Picture yourself trying to shower while your muscles burn and your heart races. Trying to get yourself clean as your body starts sweating profusely - actively working against you. You would be exhausted and frustrated.
That’s our reality every single day. We run a marathon whenever we are upright. The fatigue you feel after an intense workout? We start and end our day that way. Anything we have to do that’s vertical involves a careful energy calculation. If I need to shower - it likely means I can’t cook. If I cook - I may not be able to eat. If I have to attend a medical appointment and be upright for hours? I’m completely bedridden for days.
This is POTS. It’s not ‘JUST’ a high heart rate and ‘SOME’ tiredness.
Image Description: Blue and white infograph that shows the outline of a human body with text explaining how Dysautonomia impacts each bodily system. There’s bold orange text that says “Symptoms can be sudden and unpredictable in onset”. Bodily systems displayed are pupilomotor, neurological, pulmonary, cardiovascular, urinary, orthostatic intolerance, gastrointestinal and secretomotor. Image courtesy of The Dysautonomia Project.
Given the far reaching nature of the condition - there is no ‘quick fix.’ There’s no cure or single medication that will eliminate symptoms. Instead there’s a myriad of medications and supplements that will act as bandaids - and lifestyle modifications to hopefully improve quality of life.
How Do You Treat POTS?
Many of us start with increased salt and fluids. Your doctor will hopefully prescribe a target amount of sodium to consume each day - but suffice it to say we need a TON of salt. I drink 6-8 litres of water every day with 8-10 grams of sodium. I also consume two electrolyte mixes to ensure I’m getting enough potassium. My urine is frequently monitored to confirm I’m maintaining the proper ratios - and as you can imagine - I can never be far from a toilet. When you have to drink THIS much - you basically chain yourself to the bathroom.
Compression garments can also help. Many patients start with lower leg compression socks and graduate to thigh high and/or abdominal binders. These articles of clothing help reduce fainting by forcing the blood back up towards your heart and brain. If you have EDS you may struggle with compression - I had to stop wearing them because of severe bruising and injuries. But if you can tolerate them - they’re a great tool.
I had an OT (Occupational Therapist) assess my apartment and make modification suggestions for my safety. Simple things like a railing in the shower and raising my toilet seat an inch have had a huge impact. Not having to squat as low when getting on and off the toilet has reduced my falls (and we should all have something to grab onto in the shower).
I also have a shower chair so I can sit down when I get too dizzy. It was hard to accept that I had lost the ability to do something so simple - that I couldn’t even get through a five minute shower without assistance. But as hard as it is to accept - it was necessary to come to terms with it and purchase a chair. The shower is one of the most dangerous places you can faint - and anything you can do to reduce the risk is worth it.
I have water bottles stashed all over my apartment. Hidden in corners and on every piece of furniture because I never know WHEN or WHERE I might faint. When I pass out - I can’t get up until I’ve consumed at least 500ml of water. If I try and get up before drinking - I simply pass out again. It has been so impactful to ensure there’s always a water bottle within my reach.
Other things that can help reduce symptoms:
Reducing large and high carb meals. Digestion requires a lot of blood flow and we don’t have it to spare.
Medications like beta blockers can be used to lower heart rate - though they are contraindicated in people with low blood pressure like me
Medications to retain fluid and increase blood pressure are frequently prescribed. Fludrocortisone and Midodrine are considered first line treatments
Exercises (when safe) to strengthen your muscles can help. The stronger your muscles are the more effective they will be at pushing blood back to your heart and head (swimming and recumbent exercises like biking and rowing are great options)
Avoid infection. People with POTS can be higher risk of complications from viral and bacterial infections. A cold has put me in the hospital - usually due to my body’s inability to manage my blood pressure. Infections can also worsen the symptoms of POTS
Never be afraid to sit down. If you feel the warning signs of a faint - get to the floor. It’s always better to go to the floor voluntarily versus having your body force you
If you have EDS and/or are prone to injuries - consider getting supportive braces you can wear to help when you fall. I wear wrist splints whenever I’m doing a high risk activity or feeling particularly unstable (I started this after a fainting spell left me with a grade three wrist sprain that took nearly a year to heal)
It’s a challenge learning to exist in a world meant for people who can stand upright.
It’s hard adapting your life to accommodate being horizontal the vast majority of the time. But it CAN be done. It takes hard work and a bit of creativity - but the more you learn to lean into the condition and help your body the easier things will become.
We desperately need more awareness and advocacy around POTS and Dysautonomia - as patients are waiting far too long for diagnosis and treatment. We need more doctors who are willing to experiment and help POTS patients - and we need more people speaking out about their experiences so that patients might recognize the signs themselves.
Lastly - it’s important to learn and respect your limits. The body will give warning signals - and pushing through them never ends well. I know it’s terribly frustrating to go from being young, healthy and physically active to barely able to stand up - but denying that reality and forcing your body to do more than it’s capable of only leads to injuries and setbacks.
Be gentle. Take your time. Mourn what you’ve lost but find hope in the stories of those of us who’ve found ways to manage this insidious condition. I promise you - there IS hope. It’s just hard to see sometimes.
Never forget - you’re not lazy. You’re not a failure. POTS is exhausting and incredibly difficult to live with. Give yourself credit for getting out of bed and trying to battle through another day. Don’t let anyone tell you to push harder, exercise more or ‘suck it up.’ Listen to your body, connect with other patients and be kind to yourself. Things WILL get better.
For more on POTS - make sure you’re subscribed! Part Two will be ‘Maybe It’s Anxiety - Maybe You’ve Been Misdiagnosed’ and will focus on the LONG road to diagnosis. Part Three will be ‘Learning to Live Horizontally’ and will be a deep dive into treatments, accommodations and lifestyle modifications to help make your life as a POTSie easier.
Do you have POTS? Do you think you might have POTS? I would love to hear from you! Please like, share and leave a comment - together we can help each other learn how to manage this condition!
October is Dysautonomia Awareness Month. For events in your area - or for information on how you can help raise awareness - please visit Dysautonomia International.




I have POTS, too! I've had the symptoms for years, maybe almost a decade. It wasn't until meeting a new GP focused on chronic conditions post-pandemic that I got a diagnosis, and I think a lot of specialists would possibly write me off for not having gone to them. Because it's such an under-diagnosed and under-discussed condition, it's hard to believe that I actually have it some days (until I stand up too fast, try to take a walk, go up a few flights of stairs...). Medical fatphobia also seriously complicates POTS treatment and diagnosis, as it's easy to write off most of the symptoms as "being out of shape," to the point where there's still the persistent myth among doctors that POTS is caused by "deconditioning."
It's important to note, though, that only about 30-40% of POTS patients actually experience syncope (fainting). It's clearly a severe symptom for you, which is so important to discuss! However, I don't want people reading to think that anyone needs to faint in order to have the condition. Sometimes, fainting becomes a gatekeeping symptom in the POTS community and among doctors, so I think it's important to mention.
I have to tell you how fortunate I feel about finding you. You’ve helped me so much. I actually have a medical appointment in an hour and this article even helped me with that! I just wanted to say thank you, I’m grateful to you, and I look forward to reading your next essay in the series.