When You're Allergic to Everything and Nothing... That's MCAS
An intro guide to Mast Cell Activation Syndrome and how it has fundamentally changed my life. Living under the constant threat of anaphylaxis is hard - but there are ways to make it easier.
MCAS (Mast Cell Activation Syndrome) is arguably the condition I have which causes me the most grief. It is an absolute BEAST to manage - and poorly understood by many doctors and patients alike.
I often tell people I’m allergic to everything and nothing at all once - because I won’t test ‘positive’ on a standard IgE skin prick test yet I can (and have) had multiple episodes of anaphylaxis. Sound scary? It is. How can you possibly keep yourself safe when you’re technically not allergic to ANYTHING and yet constantly having allergic reactions?
I’m cognizant of the fact that many of my readers may not be dealing with this condition (though it is common in Long Covid) and/or may be early in their disease process and could find a ton of information overwhelming. As a result I’m going to break my MCAS pieces down into a series.
This article will be a basic introduction that I hope will be an easy read for everyone (and will tell the story of my first episode of anaphylaxis).
Part Two will explore histamine and food in greater detail, as well as mitigations like indoor air quality, cleaning products and skin care. Part Three will focus on Learning to Let Go and accept your new reality as an MCAS patient (as well as ways to cope with the stress of living under the constant threat of anaphylaxis). Let’s gently dive in… over exertion can cause a reaction!
Welcome to the world of MCAS
Your mast cells are an immune cell present all over the body and in the bone marrow. They contain histamine - but they’re also full of heparin, cytokines, leukotrienes, prostaglandin and more. When they misbehave it wreaks havoc on the body.
I have MCAS and my case has proven particularly difficult to manage. It has upended my entire life. I wish it were “just” histamine - but these pesky cells do so much more.
They see regular things such as many foods, scents, environmental triggers, sunlight, personal care products and medications as triggers… and they attack. When a mast cell degranulates it effectively explodes - and in doing so releases the chemicals mentioned above.
Given one of those chemicals is histamine - many people present with severe allergic reactions and anaphylaxis but may test negative on standard allergy testing. You’re not allergic to a specific item in the traditional sense - your mast cells are misbehaving.
Idiopathic Anaphylaxis AKA ‘I Thought It Was Just the Flu’
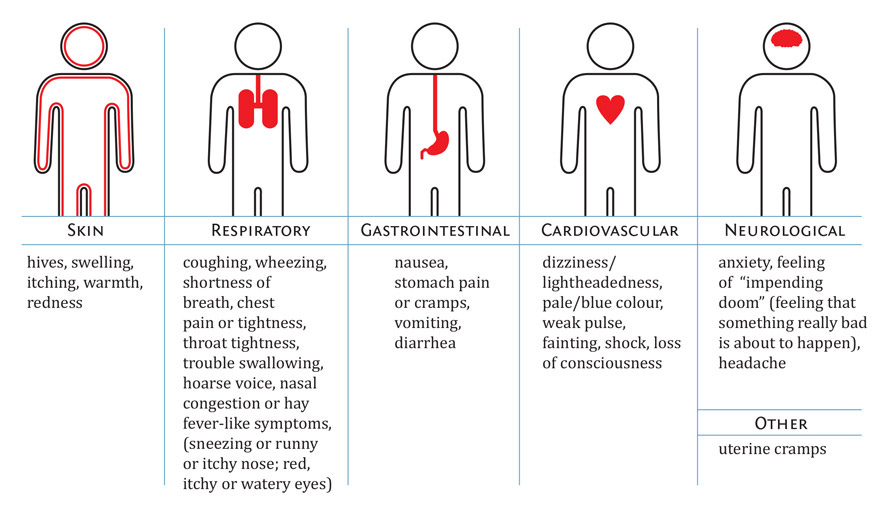
I will never forget my first episode of anaphylaxis (and how shocked I was to find out it WAS anaphylaxis). When people picture an anaphylactic reaction - they see a sudden closing of the airway rendering you unable to breathe. Did you know that’s not always the case? Anaphylaxis can impact multiple bodily systems - and sometimes the throat is completely spared. Mine impacted my gut and heart and took nearly 48 hours to progress to throat swelling.
I had diarrhea and vomiting, dizziness, tachycardia, low blood pressure and a sore throat. I thought it was the flu. I finally went to the ER on the third day because I couldn’t manage the dehydration - and I was shocked when the triage nurse panicked and rushed me into a code room.
Image Description: A chart showing the five different systems impacted by anaphylaxis and the types of symptoms you could see. The systems are skin, respiratory, gastrointestinal, cardiovascular and neurological with an ‘other’ category that lists uterine cramps. Chart courtesy of Food Allergy Canada.
Turns out I was losing my airway - that’s why my throat was “sore”. It was swelling but it was doing it at a glacial pace so I didn’t realize it was happening. My gastrointestinal and cardiac issues were the early warning signs of anaphylaxis. I was treated and sent on my way with Epi-Pens for future events (once you’ve had anaphylaxis once you will unfortunately likely have it again).
I never figured out what the trigger was. I hadn’t done anything differently, eaten any new foods or started new meds. It just happened. I was told it was idiopathic anaphylaxis (ie no known cause) and cautioned to watch for those symptoms and seek medical help sooner.
Basically - this would be my new existence. Going into anaphylaxis - a life threatening condition - at random times for absolutely no reason. It wasn’t the news I had hoped for. The flu would have been better.
Because of the strange way it presents - MCAS is often poorly understood. Many healthcare workers only consider anaphylaxis when a person has lost their airway. It’s a terrifying condition - your body betrays you. You don’t know why and if you need care they may not understand it either. In a way I’m ‘fortunate’ I waited so long to go to the ER - because had I presented earlier they might have missed the anaphylaxis and also assumed it was the ‘flu’. It was the airway issues that tipped them off and they were absent for at least two days.
Image Description: A multi coloured photo of a mast cell against a black background. There’s a purple block to the left with white text that says ‘Mast Cells are Beautiful’ The Mast Cell Disease Society. Image courtesy of TMS for a cure.
I’ve had to overhaul my whole life due to my MCAS. My diet is restricted to approximately 10 foods - all low histamine. It doesn’t stop there though - how you prepare the foods matters. Leftovers? Forget it. Food increases in histamine every second it sits uneaten.
Canned or processed foods? Same thing. Far too high in histamine and mast cells hate preservatives. So I find myself incredibly disabled and yet limited to only fresh food that can be prepared and eaten right away. It’s exhausting. Many days it’s impossible and I either don’t eat or have to rely on someone else to prepare my food for me.
The GI issues that accompany MCAS only further compound this problem. Imagine being crippled by fatigue and wasting whatever limited energy you have on cooking a bland boring meal. Then as soon as you try and eat you start vomiting or having gastric distress. You would quickly want to stop even TRYING to cook and eat.
That’s the cycle of MCAS
The exertion from cooking can be a trigger. The scents and smells of cooking can be a trigger. The heat or the strain of standing can be a trigger. But guess what else is a trigger? Hunger. Low blood sugar. You know how people joke that they’re ‘hangry’? If you’ve got MCAS you may find that ‘hangry’ quickly progresses to a full blown attack. You really can’t win.
There’s so much more to it than just food - I would need to write multiple articles to cover it all. Some of my worst episodes have been caused by neighbours smoking or cleaning their apartments, issues with my heat or AC or changes to medications or weather.
Even medications to TREAT the condition will often be a trigger. It sounds counterintuitive but unfortunately that’s how sensitive mast cells can be. Even when you’re trying to calm them you could be triggering them with an additional ingredient or dye in the medication.
As such you can never start more than one medication at a time (or you won’t know which one triggered you) and you often need everything compounded. Again it’s exhausting and expensive. Even when you do everything right there will be days you flare and never know the cause.
You Must Get Comfortable With Not Knowing
Staying ahead of my mast cells is a full time job. I understand most of my triggers quite well and can avoid them through lifestyle and dietary changes combined with restricted living. It means I have almost no life as I MUST control my environment at all times.
Even with these changes - I still experience flares quite regularly. While the initial response is often histamine based (think hives, wheezing, runny nose, itching etc) sometimes my reactions will be excessive bruising (due to heparin), flu like symptoms, bone pain, cardiac issues (low blood pressure and tachycardia) or gastrointestinal issues like diarrhea, nausea and vomiting. Mast cells can and do cause a wide range of symptoms.
Basically it’s a constant guessing game no matter how knowledgeable you are or how many sacrifices you make. You really do have to get comfortable with not knowing. You have to learn to accept that sometimes you will get incredibly sick and have no idea why. You have to find a way to let go. Trying to nail down every trigger is an exercise in futility and the stress of analyzing and over analyzing every situation can (irony of ironies) also cause an attack. Part Three in my MCAS series will be an article about mindfulness, meditation and the art of letting go - because learning to stop trying to solve every reaction was crucial for my quality of life.
Avoid Infections at All Costs
While it’s true that there will be many reactions without a known cause - infections will almost always anger the mast cells. This can be anything from something minor like a skin or tooth infection - to Covid. I have to work hard to avoid Covid infections as the virus is known to trigger MCAS in some people - and the risk is higher for those with EDS (like me).
I am unfortunately allergic to most respirators - I can only wear them for short periods of time before my face begins to swell and I develop airway issues. Given society has completely given up mitigating, isolating or trying to prevent Covid - my life has become very small.
I don’t want it to sound like it’s all doom and gloom. There are things that can help. Histamine blockers (referred to as H1s and H2s) are usually first line treatments - Quercetin is a good natural alternative. There are prescription mast cell stabilizers like Cromolyn Sodium and Ketotifen but they can be expensive and difficult to get covered by insurance.
Switching to a low histamine diet and avoiding leftovers and slow cooked meals can make a big difference. Freeze food right away and get meat and fish flash frozen. Switch to natural and unscented skin care, laundry detergent and dishwashing supplies. Get air purifiers for your home and reduce the use of chemicals that could degrade air quality.
Everything you do to lower the overall burden on your body WILL make a difference. But it is a sacrifice - I sacrifice every single day. So if someone is criticizing you for needing to order delivery, or for asking them to avoid scented products, or for isolating to avoid covid … just remember they don’t understand.
They can’t possibly fathom what it’s like to live under the constant threat of anaphylaxis, to wake up covered in bruises for no reason or to starve for weeks on end because your body can’t tolerate any food. They won’t get it unless it happens to them.
Stand firm in your choices and know that protecting your health HOWEVER you need to is never the wrong choice. When you have the energy - try and educate others so that this insidious condition gets more recognition and awareness. And be kind to yourself - it’s very hard to live with MCAS.
This post will be the first in a series of posts about Mast Cell Activation Syndrome. Subscribe below to get Part 2 - MCAS and Histamine: Diet Isn’t The Only Answer and Part 3 - Learning to Let Go: A Guide to Accepting MCAS Reactions.
Is there something about MCAS that you’ve always wanted to know? Do you want a topic covered in its own article? Do you think you might have MCAS but you’re unsure where to start? Comment below - I would love to hear from you.
If you’re struggling with MCAS (or any other disease of the mast cells) I highly recommend checking out The Mast Cell Disease Society. Their website has an abundance of resources to help patients, doctors and caregivers. Their ER guide is something I think ALL patients should have filled out and readily available for medical emergencies.



BBT, just want to say how much I appreciate your writing. Your essays are clear, lucid, direct, and powerful. Every sentence advances the reader’s understanding. And your tone is a miracle of balance. You are a terrific resource, and I believe that you undoubtedly are helping many more people than you will ever know. Thank you!
I'm so sorry about this, BBT. We found out when I as a toddler that I am deathly allergic to horses (we had 2 and my grandfather was going to get me a pony and carriage...thanks for the crap genes, dad). In my late 20s, I developed an anaphylactic reaction to aspirin and its brethren. I can only take Tylenol. I haven't been stung by a bee in ages, but I wonder, Will I have my Epipen with me the day I do? Because, with me, who knows? Wasn't allergic before. Will I be now? My terrible "specialist" pediatrician said I would "outgrow the allergies". Sure, Conrad. All the old ones have stayed and new ones to pop up. I hope the trigger(s) can be found. It took me ages to understand it was aspirin. And then it was a doctor who gave me an aspirin product (after I told her about my allergy), and that caused the anaphylactic reaction. And this was before I had an Epipen, because horses are kind of easy to avoid. LOL. Hope you're feeling better. xo